Master the art of drug safety with our expert guide on Good Clinical Practice in Pharmacovigilance. Discover essential GCP guidelines that elevate your pharmacovigilance practices and ensure top-notch compliance. Stay ahead in drug safety and regulatory excellence with our comprehensive insights.
Understanding Good Clinical Practice in Pharmacovigilance
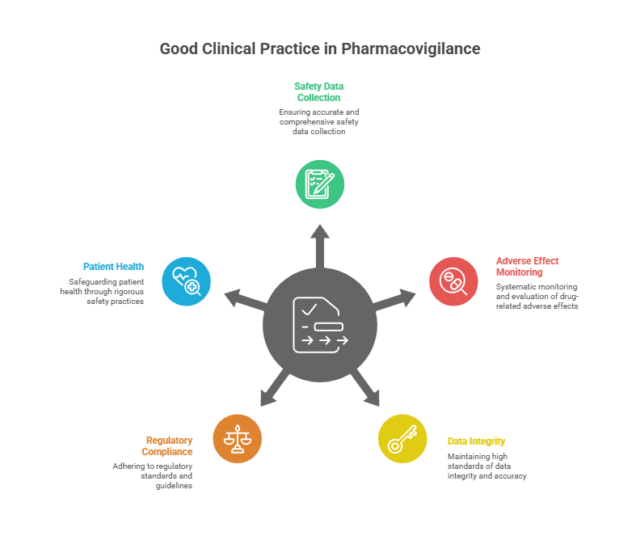
Good Clinical Practice in Pharmacovigilance is essential for ensuring the safety and efficacy of medications. Adhering to GCP guidelines in pharmacovigilance involves systematic monitoring and evaluation of drug-related adverse effects, ensuring that all safety data is accurately collected and reported. This practice safeguards patient health by maintaining high standards of data integrity and regulatory compliance, ultimately contributing to the development of safer and more effective pharmaceutical products.
What is gcp compliance
GCP compliance refers to adhering to the internationally accepted ethical and scientific quality standards for the conduct of clinical trials, Good Clinical Practice (GCP), during all aspects of clinical trials or research. GCP compliance protects the rights, safety, and welfare of study participants while ensuring the integrity, quality, and reliability of data collected in the clinical trial/study. Following GCP requirements means that you have adhered to the approved protocol; ensured proper informed consent of participants; had proper documentation; trained study staff; and met regulatory and ethical requirements through the conduct of the clinical trial/study.
Key Principles of Drug Safety Compliance
Drug safety compliance is crucial for ensuring the well-being of patients and the integrity of clinical trials. Adhering to the principles of good clinical practice in clinical research is fundamental in this process. These principles include
Rigorous Adherence to Protocols: Follow study protocols meticulously to ensure consistency and accuracy in clinical trials.
Comprehensive Monitoring and Reporting: Track and report adverse events thoroughly to maintain patient safety and data integrity.
Transparency and Accountability: Maintain clear and open documentation and reporting practices to enhance regulatory compliance.
Adherence to GCP Guidelines: Implement principles of good clinical practice to uphold high safety standards and ethical research conduct.
By following GCP guidelines, pharmaceutical companies and researchers can uphold high standards of safety, enhance regulatory compliance, and ultimately contribute to the effective and ethical development of new medications.
Essential GCP Guidelines for Pharmacovigilance
Good Clinical Practice guidelines are essential for ensuring the safety, efficacy, and quality of drugs through effective pharmacovigilance. Here are the essential GCP guidelines that play a significant role in pharmacovigilance:
- Adherence to Ethical Standards: Ensure patient safety and rights are protected throughout clinical trials and post-marketing surveillance.
- Quality Data Management: Maintain accurate, complete, and verifiable data in line with good clinical practice guidelines to enhance data reliability.
- Risk Management: Identify, assess, and manage risks associated with drug safety to prevent adverse drug reactions.
- Regulatory Compliance: Align pharmacovigilance processes with international regulations and good clinical practice guidelines for seamless operations.
- Effective Communication: Ensure clear and timely communication of safety information between stakeholders, including regulatory authorities.
- Continuous Training: Regularly train personnel involved in pharmacovigilance on the latest GCP and regulatory updates.
- Robust Documentation: Maintain detailed records of all pharmacovigilance activities as per good clinical practice guidelines for transparency and traceability.
Implementing these essential Good Clinical Practice guidelines ensures a robust pharmacovigilance system that safeguards public health.
How to Implement GCP Standards in Pharmacovigilance
To implement GCP standards in pharmacovigilance, organizations need to establish robust systems and processes for monitoring, assessing, and reporting adverse drug reactions (ADRs). This begins with training personnel on Good Clinical Practice guidelines and pharmacovigilance practices to ensure compliance with regulatory authorities like the FDA, EMA, and CDSCO. The process includes setting up a qualified team, creating standard operating procedures (SOPs) for case processing, signal detection, risk assessment, and periodic safety update reports (PSURs). Additionally, using validated software tools for data collection and analysis is crucial to maintain data integrity and traceability, which are core principles of GCP. By following these practices, pharmaceutical companies and clinical research organizations can enhance patient safety, minimize risks, and build trust with healthcare professionals and patients.
Common Challenges in Drug Safety Compliance
Drug safety compliance is essential for monitoring adverse drug reactions (ADRs) and protecting patient safety. Pharmaceutical companies must adhere to stringent regulations set by global authorities like the FDA, EMA, and WHO. However, challenges such as data management, evolving regulations, and integrating new technologies make compliance complex. Addressing these issues is vital for maintaining regulatory standards and ensuring safe and effective medications.
Challenges in Drug Safety Compliance:
- Managing large volumes of adverse event data and ensuring data accuracy.
- Adhering to constantly evolving global regulatory requirements.
- Ensuring timely and precise reporting of drug safety information.
- Integrating advanced technologies like AI and machine learning.
- Maintaining robust pharmacovigilance systems and processes.
- Coordinating efforts across multiple stakeholders and departments.
- Continuous training and upskilling of pharmacovigilance teams.
Best Practices for Adhering to GCP in Pharmacovigilance
Adhering to Good Clinical Practice (GCP) in pharmacovigilance studies is crucial for ensuring patient safety and maintaining data integrity throughout clinical trials. Key best practices include robust training for all personnel on GCP guidelines, implementing efficient and compliant reporting systems for adverse events, maintaining meticulous documentation, and ensuring proper informed consent processes. Regular audits and updates to standard operating procedures (SOPs) are essential to comply with evolving regulations. Organizations must foster a culture of quality and compliance to effectively monitor and evaluate the safety profile of investigational drugs, thereby upholding ethical standards in clinical research.
The Role of Regulatory Agencies in Drug Safety Compliance
Regulatory agencies play a crucial role in ensuring drug safety compliance by setting stringent guidelines and standards for pharmaceutical companies to follow. These agencies, such as the FDA, EMA, and CDSCO, oversee the entire drug development process, including clinical trials, manufacturing, labeling, and post-marketing surveillance, to protect public health. They ensure that drugs on the market are safe, effective, and of high quality by conducting regular audits, reviews, and inspections. Compliance with these regulations is essential for pharmaceutical companies to avoid penalties and maintain market approval for their products.
Case Studies: Effective GCP Implementation in Pharmacovigilance
Effective Good Clinical Practice (GCP) implementation is crucial in pharmacovigilance to ensure patient safety and data integrity. Case studies highlight successful GCP applications, demonstrating how robust protocols, staff training, and quality management systems lead to enhanced drug safety monitoring. These real-world examples emphasize the importance of compliance, risk management, and continuous improvement in pharmacovigilance practices. By following GCP guidelines, organizations can build trust and ensure regulatory compliance, ultimately safeguarding public health. Explore these case studies to learn more about the best practices in GCP implementation within the pharmacovigilance landscape.
Tools and Technologies for Enhancing Drug Safety Compliance
Ensuring robust drug safety compliance is critical in pharmacovigilance, and leveraging the latest tools and technologies can significantly improve this process. Cutting-edge software solutions, such as safety databases and signal detection systems, help streamline adverse event reporting and monitoring. Artificial Intelligence (AI) and Machine Learning (ML) algorithms offer predictive analytics for early risk identification. Additionally, automation tools improve data accuracy and compliance with Good Pharmacovigilance Practices (GVP). Implementing these technologies ensures a robust pharmacovigilance system, ultimately safeguarding patient health and maintaining regulatory compliance.
Future Trends in GCP and Pharmacovigilance
As the field of clinical research evolves, future trends in Good Clinical Practice (GCP) and pharmacovigilance are set to transform the landscape significantly. Advancements in technology, such as AI and machine learning, are expected to enhance data analysis and risk assessment, leading to more efficient and accurate safety monitoring. Increased focus on patient-centric approaches and real-world evidence will drive the development of more robust safety protocols and regulatory frameworks. Embracing these trends will be crucial for professionals in GCP and pharmacovigilance to stay ahead in ensuring the safety and efficacy of clinical trials and marketed products.
Recent Posts
- Global Signal Detection Trends Transforming Drug Safety 2026 March 4, 2026
- How Medical Writing Services Shapes Clinical Research, Regulatory Compliance, and Patient Communication November 6, 2025
- EudraVigilance Setup & Maintenance – Smart, Scalable Solutions June 6, 2025
- Benefit Risk Management in Pharmacovigilance for Better Drug Safety April 17, 2025
- Safety Management Plan in Pharmacovigilance for Pharma Companies Ensuring Safety April 15, 2025
Categories
Archives
FAQ's
1. What is the main purpose of good clinical practice (GCP)?
Answer: The primary goal of Good Clinical Practice (GCP) is to guarantee that clinical trials are performed ethically, safely, and scientifically. This not only safeguards the rights, safety, and welfare of participants but also ensures that the data gathered is trustworthy, precise, and dependable.
2. What is the role of gcp in pharmacovigilance?
Answer : GCP promotes pharmacovigilance by guaranteeing that clinical trials are carried out ethically and safely. It emphasizes the importance of accurately reporting and documenting any adverse events. This process aids in producing trustworthy safety information to evaluate the risk-benefit ratio of a medication.
3. What are the three main GCP principles?
Answer : Good Clinical Practice (GCP) has three main principles is the rights, safety, and well-being of participants; scientific integrity and compliance with an approved protocol; and ethical behavior through obtaining informed, voluntary consent from all participants.

